Early in his PhD program, Alphonsus Ng was tasked with finding a way to miniaturize clinical immunoassay analyzers to the size of a credit card.
“These analyzers are bulky, expensive machines that measure specific analytes in blood,” the University of Toronto graduate explains. “As part of my doctoral work, I was working with Abbott Laboratories to develop the future of that technology.”
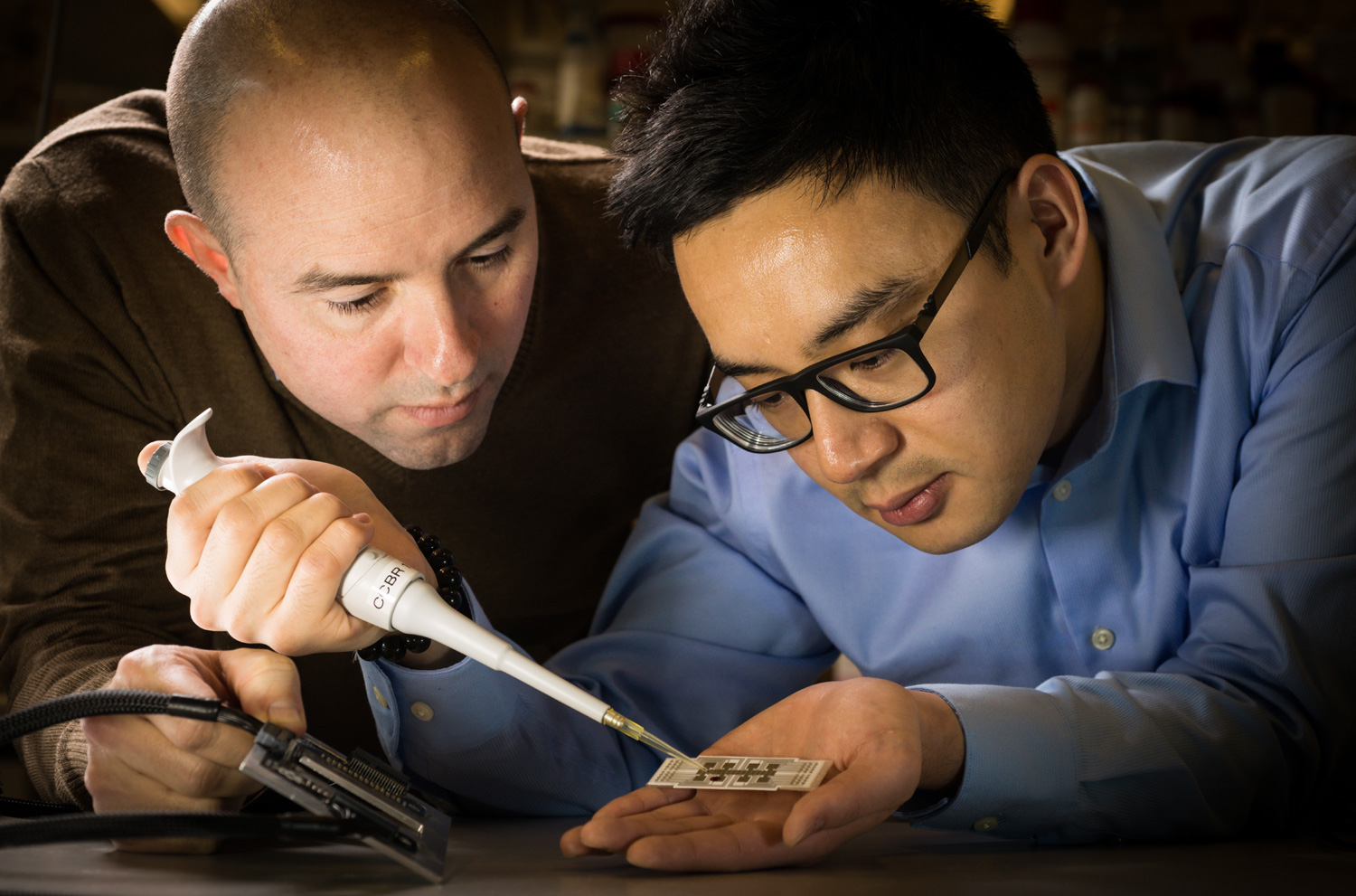
Thanks to his supervisor, digital microfluidics innovator Aaron Wheeler in U of T’s Department of Chemistry and Institute of Biomaterials and Biomedical Engineering, Ng was given a solid foundation to tackle this challenge.
Digital microfluidics is a technique used to manipulate tiny droplets of liquid on an electrode-embedded microchip. It enables researchers to carry out precise laboratory procedures faster and on a vastly smaller scale.
Over the next several years, as an NSERC Graduate Scholar, Ng developed a digital microfluidic method to separate magnetic particles from multiple droplets in parallel. Magnetic particle separation is the basis of many laboratory assays, including immunoassays. Being able to do this reliably in a miniaturized format is a game-changer.
“The great thing about this technique is that it is highly adaptable,” he says. “With the right particles and reagents, you can program the same microchip to test for virtually any diseases.”
Ng credits CMC for giving him the tools to create his solution. “They provided access to COMSOL modeling software, which allowed us to determine a magnet design to hold those particles in place for separation.”
Working with Abbott Laboratories and Ryan Fobel, CEO of Sci-Bots Inc. and a fellow doctoral student at the time, Ng and his team designed and tested a benchtop diagnostic prototype in the laboratory, and then they set themselves an even more ambitious goal.
“We wanted to build something smaller, less expensive that could run from a laptop power supply, and show that it can work outside of the lab.”
Backed by a $112,000 Grand Challenges Canada grant, the group developed their platform, dubbed the MR Box—a point of- care disease monitoring system to detect immunity to measles and rubella, infectious diseases that can be fatal to non-vaccinated children.
Working with the U.S. Centres for Disease Control and Prevention (CDC) and other international agencies, and in just three weeks, the away team tested hundreds of children and their caregivers at the Kakuma Refugee Camp in Kenya, after a camp-wide immunization campaign. Validation through traditional lab testing showed their test to be 86 per cent and 91 per cent accurate, respectively, in detecting immunity in measles and rubella samples.
‘The great thing about this technique is that it is highly adaptable’
Dr. Ng’s work was published in the illustrious journal Science Translational Medicine, and his 27 publications have been cited more than 1,500 times.
Today Dr. Ng holds a prestigious Government of Canada Banting Postdoctoral Fellowship in the laboratory of James R. Heath, first at the California Institute of Technology, and now at the Institute for Systems Biology in Seattle, WA, where he is developing microfluidics for cancer immunotherapy applications. He was also recently awarded CMC’s Douglas R. Colton Medal for Research Excellence.
It was Ng’s experience of taking his technology into the field that resonates most. “It was a unique opportunity,” he says. “Every step of the way there was some hurdle that we were able to overcome as a team. It’s something I can never forget.”
Photo: NSERC
April 2019